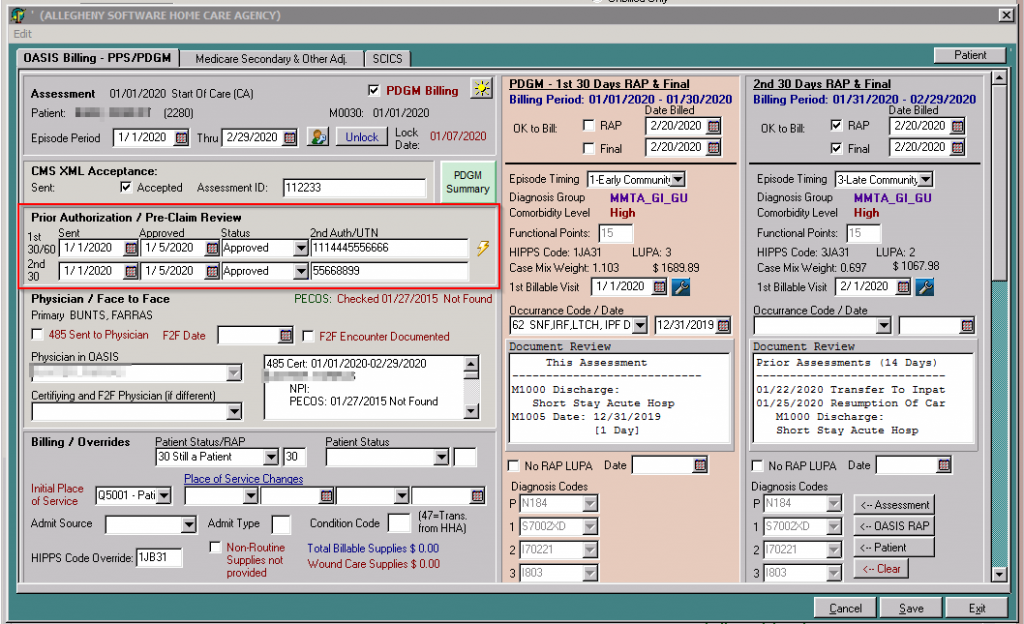
 For agencies in select states that are required by CMS to perform the Review Choice Demonstration, and participate in the Pre-claim Review Choice, Allegheny Software has added a 2nd spot for the Pre-Claim Review Choice Authorization number, as each 30-day period within home health will be eligible for review. Users will see these both within the Assessment/View/Changes button, and also within the ‘OASIS Billing Info’ Screen.
For agencies in select states that are required by CMS to perform the Review Choice Demonstration, and participate in the Pre-claim Review Choice, Allegheny Software has added a 2nd spot for the Pre-Claim Review Choice Authorization number, as each 30-day period within home health will be eligible for review. Users will see these both within the Assessment/View/Changes button, and also within the ‘OASIS Billing Info’ Screen.
This is included in Software Version 6618.
